
Dealing with workers’ compensation claims isn’t always as straightforward as one might hope. Unfortunately, as an employer, sooner or later you will have to deal with an employee injury. To help you through the process, here is a breakdown of some of the common concerns employers have while working through claims.
Independent Medical Examinations (IME)
Your workers’ compensation insurance carrier is entitled to schedule an independent medical examination, or IME. They may choose any doctor, chiropractor or psychologist. Usually, the adjuster chooses a doctor who specializes in the worker’s injury. The examination may be scheduled at any time during the claim. Once the worker is properly notified of the appointment, he or she must attend. Failure to attend places their claim on hold. Few doctors are willing to perform these examinations. They are in private practice and are not on the staff of the insurance company. Therefore, it may take a few weeks to get an appointment.
Why is an IME Scheduled?
Early in a claim, there may be a question if the injury is work-related. Is the injury a pre-existing condition? Did work actually cause the condition? Is the medical condition directly related to something at work? When these issues arise, adjusters schedule the IME soon after the claim is submitted.
Later in the claim, the adjuster may feel it’s time for the worker to return to modified or regular work. When treatment seems to drag on, an IME may be scheduled. Perhaps the worker had a new, non-work accident. An IME may help sort the work condition from the non-work condition. If the treating doctor awards permanent disability higher than normally expected, an IME may be used to see if the rating is appropriate.
An IME may be scheduled more than once on a claim. The insurance carrier is entitled to examinations at reasonable intervals. If you are concerned about any of these issues and think an IME might help, speak to us or your adjuster.
What is nurse case management?
With nurse case management, when an employee is injured, a nurse is available via 24-hour hotline to assist the employee on how to properly care for the injury. Nurses intercept the claim at the point of injury to ensure that employees obtain the right type of care from cost-effective providers. In severe cases, a nurse will recommend emergency care. With minor injuries, they are able to guide an employee through first aid and self-care treatment, or send the employee to an occupational clinic or the employer’s preferred provider network.
What benefits does it offer?
- With immediate medical advice available for employees, insureds may be able to reduce the frequency or severity/duration of workers’ compensation claims, ultimately lowering the cost of workers’ compensation insurance premiums.
- Nurses can triage injuries to the most appropriate level of care, assessing and assigning a degree of urgency to a wound or illness. By making professional decisions about treatment, the service helps contain claims costs by minimizing, for example, unnecessary visits to the emergency room.
- Claims are reported on time, avoiding penalties.
- The hotline handles required paperwork, ensuring consistent, complete record keeping and claim filing.
- Return to work coordinators receive immediate notification of the claim, allowing them to send a job description to the treating physician, who can use the information to make a more informed and accurate decision on whether to release the employee to full or modified duty.
- Efficient treatment accompanied by prompt and open communication minimizes dissatisfied injured employees, and consequently decreases costly workers’ compensation litigation.
Workers’ Compensation Hearing Applications
Workers, employers or insurance companies may file a hearing application to resolve workers’ compensation disputes. Most hearing applications are filed by workers. The application notifies the state of a dispute and initiates the legal process. A copy is forwarded to the employer and notifies them of the dispute. The application explains the claim in general. The claim may be for additional lost time, additional permanent disability benefits, penalties or unpaid medical expenses. Most workers are represented by an attorney, but they are allowed to proceed without representation if they wish.
Applications are delivered by mail. If you receive a hearing application, contact your adjuster immediately. An answer must be filed within a specified time period of the mailing. Many applications can be handled and resolved by the adjuster. More complex applications are referred to a defense attorney. The adjuster and defense attorney represent you. They should keep you informed throughout the legal process. You may contact them at any time. Your calls display your concern in the matter and can provide important information needed to defend the claim.
Hearings
Once the application is filed, the state allows time for the parties to submit their proof. After a time, the state will schedule a hearing. You will receive a Notice of Hearing six to nine months after the application is filed. The date of the hearing is two or three months following Notice of Hearing. Most hearings take four hours. A company representative should attend the Hearing to display your concern. Also, workers tend to be more accurate in their testimony when you are present. The judge’s ruling is usually rendered within 30 to 90 days. Therefore, it can take close to a year to go through the legal process. Some cases require more than one hearing and can take longer. Cases can be settled any time during the process. Settlement often occurs within 30 days of the hearing date.
What do I pay a Worker on Modified Duty?
A worker has been off due to a job-related injury. Their doctor says they can return to modified duty, and you have identified a job. When the doctor limits the number of hours a worker can be at work, you offer work up to that limit. What should they be paid?
You could pay the worker their normal rate while on modified duty. The advantage is they are being paid by you. If they work a normal week, insurance payments end. The disadvantage is that you are probably paying more than the modified duty is worth. It removes the incentive to return to normal work. This can affect the morale of co-workers.
Another option is to pay the rate for the job being done. This may be less than the worker’s regular pay, motivating the worker to return to their regular pay promptly. Most union contracts allow employers to place a worker into modified work. If your contract does not allow this, you may wish to bring this up at the next negotiation. The contract may address which jobs may be considered, how long they are available, and the wage while on modified duty.
How is the Worker Paid?
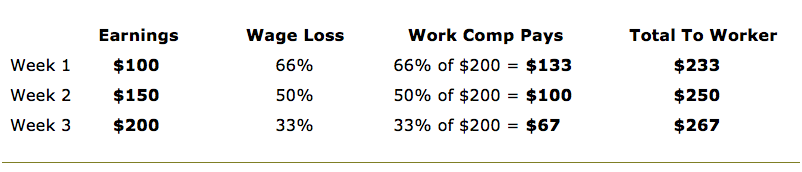
It is best to work through an example. Let’s assume the worker earns $300 per week. Compensation benefits while completely disabled are $200. What happens when you bring the worker back? The more they earn, the more they take home and the less work comp pays!
Print this Page | Contact us

